Pain In The Arches Causes Symptoms And Treatments
Foot arch pain, or pain on the bottom of the foot can be caused by a number of problems. The arches of the foot control how the forces associated with activities like walking are transferred up and down the leg. If there is a problem with the foot arches or surrounding soft tissues, pain can be felt anywhere from the foot, to the knee, to the lower back. Arch foot pain is also common when standing or walking for long periods. This is often due to weakness and tightness is the muscles and tendons which support the foot arches.
Causes
Plantar fasciitis, another sports injury detailed on this website, is regularly the cause of foot arch pain or strain. This can arise due to faulty biomechanics in your feet, which alone can also provoke foot arch pains. The most prominent biomechanical difficulties are flat feet and high arches. With flat feet (or overpronation) the arches appear to be almost flattened, causing unevenness by forcing the feet roll inwards in order to maintain balance and support the body's weight. This places inordinate pressure on the plantar fascia and arches. If by contrast you have high arches (instep), the ankle can roll outwards, again causing undue strain on the arches. Too much of this strain can lead to stretching of the plantar fascia and pain in the arches. Other causes include overstretching or otherwise pressuring the arches, for example by exercising with fatigued leg muscles which leave the feet with excessive work to do. You are also particularly at risk if in your 40s or 50s and commencing an intense program of training after a long period of inactivity.
Symptoms
Typically, the sufferer of plantar fasciitis experiences pain upon rising after sleep, particularly the first step out of bed. Such pain is tightly localized at the bony landmark on the anterior medial tubercle of the calcaneus. In some cases, pain may prevent the athlete from walking in a normal heel-toe gait, causing an irregular walk as means of compensation. Less common areas of pain include the forefoot, Achilles tendon, or subtalar joint. After a brief period of walking, the pain usually subsides, but returns again either with vigorous activity or prolonged standing or walking. On the field, an altered gait or abnormal stride pattern, along with pain during running or jumping activities are tell-tale signs of plantar fasciitis and should be given prompt attention. Further indications of the injury include poor dorsiflexion (lifting the forefoot off the ground) due to a shortened gastroc complex, (muscles of the calf). Crouching in a full squat position with the sole of the foot flat on the ground can be used as a test, as pain will preclude it for the athlete suffering from plantar fasciitis, causing an elevation of the heel due to tension in the gastroc complex.
Diagnosis
A patient is asked to step with full body weight on the symptomatic foot, keeping the unaffected foot off the ground. The patient is then instructed to "raise up on the tip toes" of the affected foot. If the posterior tibial tendon has been attenuated or ruptured, the patient will be unable to lift the heel off the floor and rise onto the toes. In less severe cases, the patient will be able to rise on the toes, but the heel will not be noted to invert as it normally does when we rise onto the toes. X-rays can be helpful but are not diagnostic of the adult acquired flatfoot. Both feet, the symptomatic and asymptomatic - will demonstrate a flatfoot deformity on x-ray. Careful observation may show a greater severity of deformity on the affected side.
Non Surgical Treatment
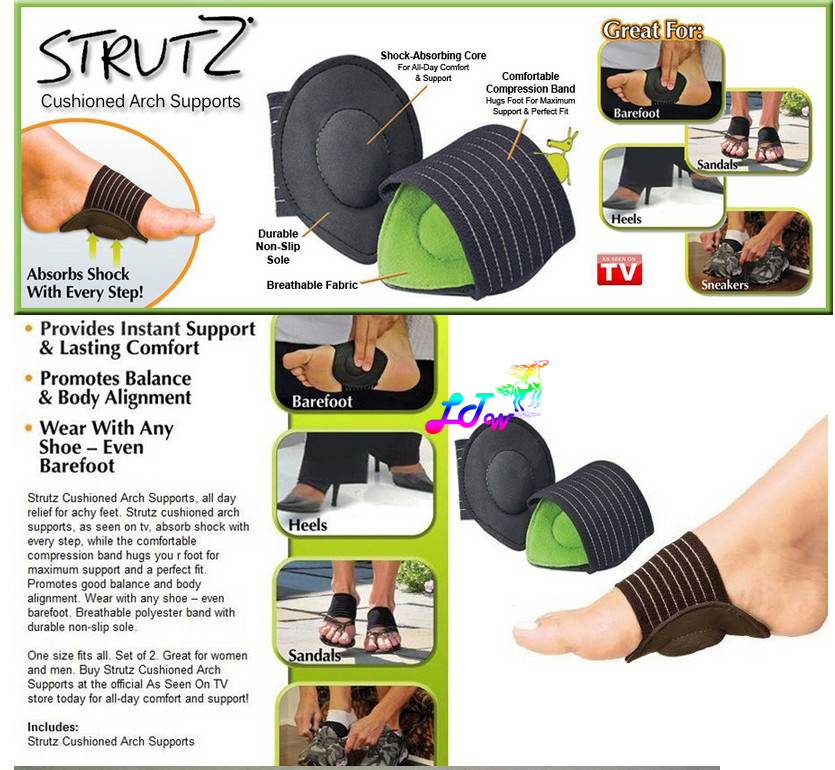
In mild cases of flatfoot the first line of treatment is often custom orthotics. In patients with a flexible deformity, supporting the arch with a custom arch support will take the strain off the joints and muscles, bringing the heel into a corrected position. Wider shoe gear may be prescribed to accommodate foot pain and motion and stretching exercises to decrease stiffness and stress on the foot. In cases of severe collapse, especially if the patient is not a good surgical candidate or has a mild tear, a brace may be made to accommodate the foot and ankle, thus supporting the arch and ankle.

Surgical Treatment
Patients with adult acquired flatfoot are advised to discuss thoroughly the benefits vs. risks of all surgical options. Most procedures have long-term recovery mandating that the correct procedure be utilized to give the best long-term benefit. Most flatfoot surgical procedures require six to twelve weeks of cast immobilization. Joint fusion procedures require eight weeks of non-weightbearing on the operated foot, meaning you will be on crutches for two months. The bottom line is: Make sure all of your non-surgical options have been covered before considering surgery. Your primary goals with any treatment are to eliminate pain and improve mobility. In many cases, with the properly designed foot orthosis or ankle brace, these goals can be achieved without surgical intervention.
Prevention
Stretch and strengthen important muscles in your feet, ankles and legs in order to guard against future strain. Make sure to acquire suitable arch supports and inserts if necessary, and that your shoes are shock absorbent and in good condition. Wearing tattered shoes provides no protection, and runners should replace their footwear before exceeding 500 miles of usage. Athletes new to arch supports should gradually build their training routine, allowing their feet to become accustomed to a new stance.
Stretching Exercises
Strengthening exercises. Below are two simple strength exercises to help condition the muscles, tendons and joints around the foot and ankle. Plantar Rolling. Place a small tin can or tennis ball under the arch of the affected foot. Slowly move the foot back and forth allowing the tin can or tennis ball to roll around under the arch. This activity will help to stretch, strengthen and massage the affected area. Toe Walking. Stand upright in bare feet and rise up onto the toes and front of the foot. Balance in this position and walk forward in slow, small steps. Maintain an upright, balanced posture, staying as high as possible with each step. Complete three sets of the exercise, with a short break in between sets, for a total of 20 meters.
Posterior Tibial Tendon Dysfunction Healing
Overview
The posterior tibial tendon serves as one of the major supporting structures of the foot, helping it to function while walking. Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch. This results in flattening of the foot. PTTD is often called ?adult acquired flatfoot? because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse, especially if it isn?t treated early. 
Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot deformity. There is often no specific event that starts the problem, such as a sudden tendon injury. More commonly, the tendon becomes injured from cumulative wear and tear. Posterior tibial tendon dysfunction occurs more commonly in patients who already have a flat foot for other reasons. As the arch flattens, more stress is placed on the posterior tibial tendon and also on the ligaments on the inside of the foot and ankle. The result is a progressive disorder.
Symptoms
Pain and swelling around the inside aspect of the ankle initially. Later, the arch of the foot may fall (foot becomes flat), this change leads to walking to become difficult and painful, as well as standing for long periods. As the flat foot becomes established, pain may progress to the outer part of the ankle. Eventually, arthritis may develop.
Diagnosis
First, both feet should be examined with the patient standing and the entire lower extremity visible. The foot should be inspected from above as well as from behind the patient, as valgus angulation of the hindfoot is best appreciated when the foot is viewed from behind. Johnson described the so-called more-toes sign: with more advanced deformity and abduction of the forefoot, more of the lateral toes become visible when the foot is viewed from behind. The single-limb heel-rise test is an excellent determinant of the function of the posterior tibial tendon. The patient is asked to attempt to rise onto the ball of one foot while the other foot is suspended off the floor. Under normal circumstances, the posterior tibial muscle, which inverts and stabilizes the hindfoot, is activated as the patient begins to rise onto the forefoot. The gastrocnemius-soleus muscle group then elevates the calcaneus, and the heel-rise is accomplished. With dysfunction of the posterior tibial tendon, however, inversion of the heel is weak, and either the heel remains in valgus or the patient is unable to rise onto the forefoot. If the patient can do a single-limb heel-rise, the limb may be stressed further by asking the patient to perform this maneuver repetitively.
Non surgical Treatment
Non-surgical treatment consists of custom orthoses and or special bracing devices along with supportive measures aimed at reducing the symptoms. While non-surgical treatment helps the majority of patients with PTTD, progressive cases may require surgical treatment including soft tissue tendon transfers, osteotomies and lastly fusion. 
Surgical Treatment
For more chronic flatfoot pain, surgical intervention may be the best option. Barring other serious medical ailments, surgery is a good alternative for patients with a serious problem. There are two surgical options depending on a person?s physical condition, age and lifestyle. The first type of surgery involves repair of the PTT by transferring of a nearby tendon to help re-establish an arch and straighten out the foot. After this surgery, patients wear a non-weight bearing support boot for four to six weeks. The other surgery involves fusing of two or three bones in the hind foot below the ankle. While providing significant pain relief, this option does take away some hind foot side-to-side motion. Following surgery, patients are in a cast for three months. Surgery is an effective treatment to address adult-acquired flatfoot, but it can sometimes be avoided if foot issues are resolved early. That is why it is so important to seek help right away if you are feeling ankle pain. But perhaps the best way to keep from becoming flatfooted is to avoid the risk factors altogether. This means keeping your blood pressure, weight and diabetes in check.
What Are The Causes Of A Ruptured Achilles Tendon?
Overview 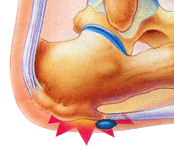 The Achilles' tendon is located in the leg just behind and above the heel. As the connection between the heel and calf muscle, its function is to allow the bending of the foot downwards. Generally if there is a tear to the Achilles' tendon it will be known as a rupture. This can be a partial tear or a complete tear, although partial tears are much rarer. Causes The Achilles tendon is most commonly injured by sudden plantarflexion or dorsiflexion of the ankle, or by forced dorsiflexion of the ankle outside its normal range of motion. Other mechanisms by which the Achilles can be torn involve sudden direct trauma to the tendon, or sudden activation of the Achilles after atrophy from prolonged periods of inactivity. Some other common tears can occur from overuse while participating in intense sports. Twisting or jerking motions can also contribute to injury. Fluoroquinolone antibiotics, famously ciprofloxacin, are known to increase the risk of tendon rupture, particularly achilles. Symptoms Although it's possible to have no signs or symptoms with an Achilles tendon rupture, most people experience pain, possibly severe, and swelling near your heel, an inability to bend your foot downward or "push off" the injured leg when you walk, an inability to stand on your toes on the injured leg, a popping or snapping sound when the injury occurs. Seek medical advice immediately if you feel a pop or snap in your heel, especially if you can't walk properly afterward. Diagnosis The diagnosis of an Achilles tendon rupture is made entirely on physical examination. Often, there is a substantial defect in the Achilles from 2-5 cm before it inserts into the heel bone. However, the main test is to determine whether the Achilles has been ruptured is the Thompson test. This essentially involves placing the patient on their stomach and squeezing the calf muscle. If the Achilles is intact, the foot will rise [plantar flex]. If it is ruptured, the foot will not move and will tend to be in a lower lying position. Non Surgical Treatment Your doctor may advise you to rest your leg and keep the tendon immobile in a plaster cast while it heals. Or you may need to have an operation to treat an Achilles tendon rupture. The treatment you have will depend on your individual circumstances, such as your age, general health and how active you are. It will also depend on whether you have partially or completely torn your tendon. If you have a partial tear, it might get better without any treatment. Ask your doctor for advice on the best treatment for you. If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
The Achilles' tendon is located in the leg just behind and above the heel. As the connection between the heel and calf muscle, its function is to allow the bending of the foot downwards. Generally if there is a tear to the Achilles' tendon it will be known as a rupture. This can be a partial tear or a complete tear, although partial tears are much rarer. Causes The Achilles tendon is most commonly injured by sudden plantarflexion or dorsiflexion of the ankle, or by forced dorsiflexion of the ankle outside its normal range of motion. Other mechanisms by which the Achilles can be torn involve sudden direct trauma to the tendon, or sudden activation of the Achilles after atrophy from prolonged periods of inactivity. Some other common tears can occur from overuse while participating in intense sports. Twisting or jerking motions can also contribute to injury. Fluoroquinolone antibiotics, famously ciprofloxacin, are known to increase the risk of tendon rupture, particularly achilles. Symptoms Although it's possible to have no signs or symptoms with an Achilles tendon rupture, most people experience pain, possibly severe, and swelling near your heel, an inability to bend your foot downward or "push off" the injured leg when you walk, an inability to stand on your toes on the injured leg, a popping or snapping sound when the injury occurs. Seek medical advice immediately if you feel a pop or snap in your heel, especially if you can't walk properly afterward. Diagnosis The diagnosis of an Achilles tendon rupture is made entirely on physical examination. Often, there is a substantial defect in the Achilles from 2-5 cm before it inserts into the heel bone. However, the main test is to determine whether the Achilles has been ruptured is the Thompson test. This essentially involves placing the patient on their stomach and squeezing the calf muscle. If the Achilles is intact, the foot will rise [plantar flex]. If it is ruptured, the foot will not move and will tend to be in a lower lying position. Non Surgical Treatment Your doctor may advise you to rest your leg and keep the tendon immobile in a plaster cast while it heals. Or you may need to have an operation to treat an Achilles tendon rupture. The treatment you have will depend on your individual circumstances, such as your age, general health and how active you are. It will also depend on whether you have partially or completely torn your tendon. If you have a partial tear, it might get better without any treatment. Ask your doctor for advice on the best treatment for you. If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.  Surgical Treatment Surgery offers important potential benefits. Besides decreasing the likelihood of re-rupturing the Achilles tendon, surgery often increases the patient?s push-off strength and improves muscle function and movement of the ankle. Various surgical techniques are available to repair the rupture. The surgeon will select the procedure best suited to the patient. Following surgery, the foot and ankle are initially immobilized in a cast or walking boot. The surgeon will determine when the patient can begin weightbearing. Complications such as incision-healing difficulties, re-rupture of the tendon, or nerve pain can arise after surgery. Whether an Achilles tendon rupture is treated surgically or non-surgically, physical therapy is an important component of the healing process. Physical therapy involves exercises that strengthen the muscles and improve the range of motion of the foot and ankle.
Surgical Treatment Surgery offers important potential benefits. Besides decreasing the likelihood of re-rupturing the Achilles tendon, surgery often increases the patient?s push-off strength and improves muscle function and movement of the ankle. Various surgical techniques are available to repair the rupture. The surgeon will select the procedure best suited to the patient. Following surgery, the foot and ankle are initially immobilized in a cast or walking boot. The surgeon will determine when the patient can begin weightbearing. Complications such as incision-healing difficulties, re-rupture of the tendon, or nerve pain can arise after surgery. Whether an Achilles tendon rupture is treated surgically or non-surgically, physical therapy is an important component of the healing process. Physical therapy involves exercises that strengthen the muscles and improve the range of motion of the foot and ankle.
Fallen Arches Causes, Indicators And Treatment Method

A fallen arch or flatfoot is known medically as pes planus. The foot loses the gently curving arch on the inner side of the sole, just in front of the heel. If this arch is flattened only when standing and returns when the foot is lifted off the ground, the condition is called flexible pes planus or flexible flatfoot. If the arch disappears in both foot positions, standing and elevated, the condition is called rigid pes planus or rigid flatfoot.
Causes
There are many different causes of flat feet, which can be separated into two main categories. The first category, congenital flat foot, is a condition that one is born with or is predisposed to at birth. This type includes the completely asymptomatic, pediatric flexible flat foot-by far the most common form of congenital flat foot. Flexible means that an arch is present until weight is put on the foot, at which time the arch disappears. This foot type is a result of the fact that all people are born with different physical features. Some people have bigger noses than others, just as some people have flatter feet (of course, there is no known correlation between the two). Any alteration in the many building blocks of the foot can influence its shape. At the other end of the spectrum, yet within the same category of congenital flat foot, exist several rare, more severe forms of flat foot. These severe conditions include Vertical Talus, Congenital Calcaneal Valgus, and Tarsal Coalitions - all of which are more rigid (no arch with or without weight on the foot) and definitely symptomatic. Luckily, these are much less common, but can usually be identified by specialists at the time of presentation and treated appropriately. The second category, acquired flat foot, develops over time, rather than at birth. Many different factors can contribute to the development of flat feet. These include the types of shoes a child wears, a child's sitting or sleeping positions, compensation for other abnormalities further up the leg, or more severe factors such as rupture of ligaments or tendons in the foot. Very commonly, the reason for flat feet is that the foot is compensating for a tight Achilles tendon. If the Achilles tendon is tight, then it causes the foot to point down, or to plantarflex (as occurs when stepping on the accelerator of your car). Even minimal amounts of plantarflexion can simulate a longer leg on that particular side, assuming that the other foot is in the normal position. The body therefore tries to compensate by pronating, or flattening out the arch, thereby making up for the perceived extra length on the affected side.
Symptoms
Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area. Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot. The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
Podiatrists are trained in expertly assessing flat feet and identifying different risk factors and the causes for it. Initial assessment will begin with a detailed history attempting to find out if any underlying illness has resulted in this. A detailed clinical examination normally follows. The patient may be asked to perform certain movements such as walking or standing on their toes to assess the function of the foot. Footwear will also be analysed to see if there has been excessive wear or if they are contributing to the pronation of the foot. To assess the structure of the foot further, the podiatrist may perform certain x-rays to get a detailed idea of the way the bones are arranged and how the muscle tissues may be affecting them. It also helps assess any potential birth defects in a bit more detail.
Non Surgical Treatment
Treatment of flat feet really depends on how far the damage has progressed. Conservative treatments often include immobilization (often by cast or brace) to reduce inflammation. Your doctor may also recommend anti-inflammatory medication (like ibuprofen) to get your inflamed tendon to calm down a bit. Orthotics can also offer significant relief. If these treatments fail to significantly improve symptoms, then surgery may be your best option to get the structure of your body back where it needs to be. Your podiatrist can discuss surgical options with you in great depth.
Surgical Treatment

A better approach is to strengthen the weakened ligaments with Prolotherapy, supplemented by an arch support if the condition has existed for several years. Chronic pain is most commonly due to tendon and ligament weakness, or cartilage deterioration. The safest and most effective natural medicine treatment for repairing tendon, ligament and cartilage damage is Prolotherapy. In simple terms, Prolotherapy stimulates the body to repair painful areas. It does so by inducing a mild inflammatory reaction in the weakened ligaments and cartilage. Since the body heals by inflammation, Prolotherapy stimulates healing. Prolotherapy offers the most curative results in treating chronic pain. It effectively eliminates pain because it attacks the source: the fibro-osseous junction, an area rich in sensory nerves. What?s more, the tissue strengthening and pain relief stimulated by Prolotherapy is permanent.
Prevention
Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches.
Pes Planus Causes, Signs And Symptoms And Treatment Solution
If you have flat feet, you may also experience pain throughout the lower body and into the lower back. Orthotics can be prescribed to create a system of support for the body and surgery can also offer a more permanent solution. Contact us today to discuss which treatment option may be right for you.
Causes
There are many different causes of flat feet, which can be separated into two main categories. The first category, congenital flat foot, is a condition that one is born with or is predisposed to at birth. This type includes the completely asymptomatic, pediatric flexible flat foot-by far the most common form of congenital flat foot. Flexible means that an arch is present until weight is put on the foot, at which time the arch disappears. This foot type is a result of the fact that all people are born with different physical features. Some people have bigger noses than others, just as some people have flatter feet (of course, there is no known correlation between the two). Any alteration in the many building blocks of the foot can influence its shape. At the other end of the spectrum, yet within the same category of congenital flat foot, exist several rare, more severe forms of flat foot. These severe conditions include Vertical Talus, Congenital Calcaneal Valgus, and Tarsal Coalitions - all of which are more rigid (no arch with or without weight on the foot) and definitely symptomatic. Luckily, these are much less common, but can usually be identified by specialists at the time of presentation and treated appropriately. The second category, acquired flat foot, develops over time, rather than at birth. Many different factors can contribute to the development of flat feet. These include the types of shoes a child wears, a child's sitting or sleeping positions, compensation for other abnormalities further up the leg, or more severe factors such as rupture of ligaments or tendons in the foot. Very commonly, the reason for flat feet is that the foot is compensating for a tight Achilles tendon. If the Achilles tendon is tight, then it causes the foot to point down, or to plantarflex (as occurs when stepping on the accelerator of your car). Even minimal amounts of plantarflexion can simulate a longer leg on that particular side, assuming that the other foot is in the normal position. The body therefore tries to compensate by pronating, or flattening out the arch, thereby making up for the perceived extra length on the affected side.
Symptoms
A significant number of people with fallen arches (flat feet) experience no pain and have no problems. Some, however, may experience pain in their feet, especially when the connecting ligaments and muscles are strained. The leg joints may also be affected, resulting in pain. If the ankles turn inwards because of flat feet the most likely affected areas will be the feet, ankles and knees. Some people have flat feet because of a developmental fault during childhood, while others may find that the problem develops as they age, or after a pregnancy. There are some simple devices which may prevent the complications of flat feet.
Diagnosis
You can always give yourself the ?wet test? described above to see whether you have flat feet. Most people who do not notice their flat feet or have no pain associated with them do not think to see a foot doctor. Flat feet can lead to additional problems such as stiffness or pain, however, especially if the condition appears out of nowhere. If you think you may have flat feet, you should seek medical attention to ensure there are no additional issues to worry about. Your doctor will be able to diagnose you with a number of tests. For example, he or she may have you walk around, stand still, or stand on your tiptoes while you are being examined. Your doctor may also examine your foot?s shape and functionality. It?s important to let your foot doctor know about your medical and family history. In some cases, your doctor may order imaging tests such as x-rays or an MRI (magnetic resonance imaging) to determine a cause of your flat foot. If tarsal coalition is suspected in children, a CT scan is often ordered.
Non Surgical Treatment
In rare cases, surgery may be needed if a child has flat feet caused by a problem they're born with (a congenital abnormality). The foot may need to be straightened or the bones may need to be separated if they're fused together. Painkillers and insoles are the first treatment options for flat feet that are caused by a joint problem, such as arthritis or a torn tendon. However, surgery may be recommended if the injury or condition is severely affecting your feet. Where flat feet are caused by a condition that affects the nervous system, special shoes, insoles, or supportive foot or leg braces may be needed. Again, in severe cases, an operation may be needed to straighten the feet.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer).
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Does Pain In The Foot's Arch Need Surgery ?
Pain across the bottom of the foot at any point between the heel and the ball of the foot is often referred to as "arch pain." Although this description is non-specific, most arch pain is due to strain or inflammation of the plantar fascia (a long ligament on the bottom of the foot). This condition is known as plantar fasciitis and is sometimes associated with a heel spur. In most cases, arch pain develops from overuse, unsupportive shoes, weight gain, or acute injury. If arch pain persists beyond a few days, see a foot and ankle surgeon for treatment to prevent this condition from becoming worse.

Causes
Unlike a flexible flatfoot, a rigid flatfoot is often the result of a significant problem affecting the structure or alignment of the bones that make up the foot's arch. Some common causes of rigid flatfeet include Congenital vertical talus, In this condition, there is no arch because the foot bones are not aligned properly. In some cases, there is a reverse curve (rocker-bottom foot, in which the shape is like the bottom rails of a rocking chair) in place of the normal arch. Congenital vertical talus is a rare condition present at birth. It often is associated with a genetic disorder, such as Down syndrome, or other congenital disorders. The cause is unknown in up to half of cases. Tarsal coalition (peroneal spastic flatfoot), In this inherited condition, two or more of the foot bones are fused together, interfering with the flexibility of the foot and eliminating the normal arch. A rare condition, it often affects several generations of the same family. Lateral subtalar dislocation. Sometimes called an acquired flatfoot, it occurs in someone who originally had a normal foot arch. In a lateral subtalar dislocation, there is a dislocation of the talus bone, located within the arch of the foot. The dislocated talus bone slips out of place, drops downward and sideways and collapses the arch. It usually occurs suddenly because of a high-impact injury related to a fall from a height, a motor vehicle accident or participation in sports, and it may be associated with fractures or other injuries.
Symptoms
Experiencing chronic pain of any kind can lead to feelings of fatigue, irritability and even depression. Friends may joke about having 'tired dogs' after a long day, but this is completely different from your experience if arch pain has begun to impact your life on a daily basis. You may dread getting out of bed in the morning and wonder how you're going to get through a work day without having to limp home at the end of it.
Diagnosis
In more difficult cases of plantar fasciitis you should see your foot health professional for a thorough examination. They will find out why your arch or heel pain occurred in the first place and devise a treatment plan to relieve your pain and prevent it from reoccurring. They will evaluate your feet, walking pattern (gait), shoes, activities, exercise methods, and other relevant information and then devise your treatment plan.
Non Surgical Treatment
The treatment is to put an arch support under the foot immediately to prevent the arch from collapsing and the plantar fascia from stretching. Also, put an arch support in your slippers and wear them as soon as you rise. Even a few steps barefoot without support can stretch the plantar fascia. Arch supports usually relieve pain within a few days. To head off arch pain, begin an exercise routine slowly, take off any excess weight and wear arch supports in your athletic shoes. Arch pain commonly smolders for months because people do not take the proper precautions. Continuing to do weight-bearing exercises will perpetuate the pain. While the foot is recovering, swim or do water workouts. Or work the upper body only. Some people are able to use a stationary bicycle by placing only the front part of the foot on the pedals.

Surgical Treatment
Surgery is considered only after 12 months of aggressive nonsurgical treatment. Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet, despite a year of calf stretches. In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope, an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low, but can include nerve damage. Plantar fascia release. If you have a normal range of ankle motion and continued heel pain, your doctor may recommend a partial release procedure. During surgery, the plantar fascia ligament is partially cut to relieve tension in the tissue. If you have a large bone spur, it will be removed, as well. Although the surgery can be performed endoscopically, it is more difficult than with an open incision. In addition, endoscopy has a higher risk of nerve damage. The most common complications of release surgery include incomplete relief of pain and nerve damage. Most patients have good results from surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after all nonsurgical measures have been exhausted.
Stretching Exercises
People with flexible feet who develop fallen arches may benefit from foot strengthening exercises, notes the Nicholas Institute of Sports Medicine and Athletic Trauma. Standing on a towel in bare feet and grasping the material with the toes is an easy foot-strengthening exercise that can be done at home. Standing on one leg while arching and releasing the foot may also prove useful. Doctors may prescribe gentle stretching exercises for the foot and ankle tendons.
Pain In The Foot's Arch Causes Symptoms And Treatments
Posterior tibial tendon dysfunction is one of several terms to describe a painful, progressive flatfoot deformity in adults. Other terms include posterior tibial tendon insufficiency and adult acquired flatfoot. The term adult acquired flatfoot is more appropriate because it allows a broader recognition of causative factors, not only limited to the posterior tibial tendon, an event where the posterior tibial tendon looses strength and function. The adult acquired flatfoot is a progressive, symptomatic (painful) deformity resulting from gradual stretch (attenuation) of the tibialis posterior tendon as well as the ligaments that support the arch of the foot.

Causes
Arch pain is most often caused by plantar fasciitis, which can affect the heel, arch, or both. Plantar fasciitis treatment is the same, regardless of the location of foot pain (see above). For persistent plantar fasciitis, an injection with a mixture of a steroid and local anesthetic can be helpful. Fallen arches or flat feet occur when the arches of the feet flatten out (often when standing or walking), causing foot pain and other problems. Flat feet can be treated with shoe inserts (orthotics), shoe adjustments, rest/ice, using a walking cane or brace, or physical therapy. Occasionally, surgery is necessary.
Symptoms
Go to a podiatrist at the first sign of symptoms. Besides pain on the bottom of the foot, additional symptoms may include burning sensation in arch, difficulty standing on tiptoes, inflammation, more pain after sleeping or resting, redness, heat, localized pain in the ball of the foot, sharp or shooting pain in the toes, pain that increases when toes are flexed, tingling or numbness in the toes, aching, pain that increases when walking barefoot, pain that increases when walking on hard surfaces, pain the increases when standing (putting weight on your feet) or moving around and decreases when immobile, skin Lesions, it?s important to get a proper diagnosis and treatment plan. Let?s go over the possible causes of the pain.
Diagnosis
The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
Non Surgical Treatment
High arches that are flexible do not require any treatment. In cases where there is pain, shoe modifications such as an arch insert or support insole can help to relieve pain during walking. Custom orthotic devices can be given that fit into the shoe and provide stability and cushioning effect. Your doctor may recommend a brace to help keep the foot and ankle stable. In severe cases, surgery is performed to flatten the foot. Any coexisting nerve disorders are also treated.

Surgical Treatment
The procedure involves cutting and shifting the bone, and then performing a tendon transfer. First, the surgeon performs a calcaneal osteotomy, cutting the heel bone and shifting it into the correct position. Second, the surgeon transfers the tendon. Reroute the flexor digitorum to replace the troublesome posterior tibial tendon. Finally, the surgeon typically performs one or more fine-tuning procedures that address the patient?s specific foot deformity. Often, the surgeon will lengthen the Achilles tendon because it is common for the mispositioned foot to cause the Achilles to tighten. Occasionally, to increase the arch, the surgeon performs another osteotomy of one of the bones of the midfoot. Occasionally, to point the foot in a straightforward direction, the surgeon performs another osteotomy of the outside portion of the calcaneus.
Prevention
The best way to prevent plantar fasciitis is to wear shoes that are well made and fit your feet. This is especially important when you exercise, walk a lot, or stand for a long time on hard surfaces. Get new athletic shoes before your old shoes stop supporting and cushioning your feet. You should also avoid repeated jarring to the heel. Maintain a healthy weight. Stretch when you feel a tightening of the ligament that runs along the bottom of your foot. Stop impact sports when symptoms first occur.
Stretching Exercises
Try these simple stretches to assist with relieving pain in your arches. (Note: Stretch slowly and gently. You should feel a moderate pull on the muscle and tendon but no pain. If these stretches are painful, stop and seek further advice from a health professional). STRETCH ONE. Stand at arm?s length from a wall with one foot in front of the other, forward knee bent. Keeping your back leg straight and back heel on the floor, lean into the wall until you feel a stretch in your calf. STRETCH TWO. This time, bend your back leg slightly, and lean into the wall. You should feel a stretch in the lower part of your calf. Hold each stretch for 20 seconds and repeat on each leg, a few times daily.